Worries and concerns about having to undergo a mastectomy due to breast cancer or related health concerns are completely understandable. The good news is that breast reconstruction surgery can help women feel whole again. This type of surgery uses artificial implants to recreate and restore the breast’s size and shape.
This type of surgery should pose a considerable number of questions to patients. Washington, D.C. doctors are equipped with the most up to date technologies and are able to provide individualized care to aid in achieving the overall desired outcome.
This type of procedure can have a dramatic impact on your overall self-esteem and day to day living. Here, we will give a description of the surgery, the targeted audience, the process of the surgery, the experience during recovery, and the expectations that one should have in Washington, D.C. Let’s keep it simple.
Table of Contents
What Is Implant-Based Breast Reconstruction?
This procedure is classified as some type of breast. Incorporating medical implants that are either filled with saline or silicone. The silicone type are softer and more pliable resembling real breast tissue. The surgical procedure is performed to create a more natural, aesthetic appearance to the breast after a mastectomy. This procedure is also referred to as silicone breast reconstruction.
It’s different from another type called “autologous” reconstruction, which uses your own skin and fat from somewhere else on your body. Implants are quicker and don’t need taking tissue from other spots.
Global Use of Implant‑Based Breast Reconstruction
Implant‑based reconstruction is the most commonly performed breast reconstruction method worldwide, especially in North America and parts of Europe, due to shorter surgery time and predictable outcomes.
Global Distribution of Breast Reconstruction Methods
| Region | Implant‑Based (%) | Autologous (%) | Combined (%) |
| North America | 75 | 20 | 5 |
| Europe | 62 | 30 | 8 |
| Asia‑Pacific | 55 | 35 | 10 |
| Latin America | 58 | 32 | 10 |
| Middle East | 60 | 28 | 12 |
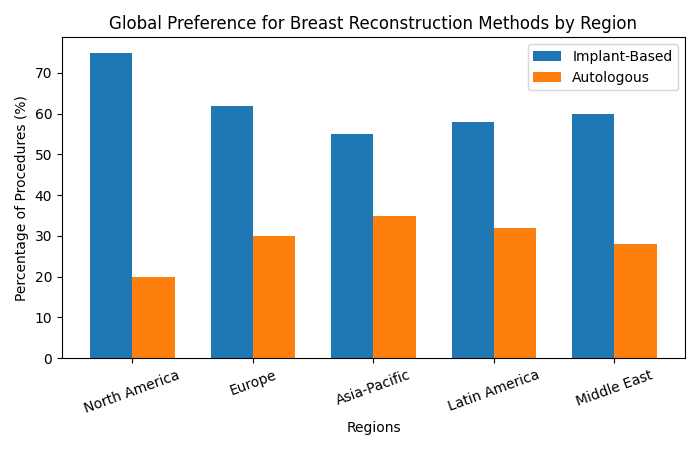
Global Preference for Breast Reconstruction Methods by Region
- X‑axis: Regions
- Y‑axis: Percentage of procedures
- Implant‑based vs Autologous
Who Is It For?
It’s great for women who’ve had a mastectomy and want their breasts back. You should be healthy overall and know what to expect—it’s not perfect, but it helps a lot. Talk to a plastic surgeon to see if it’s right for you. They’ll check your health and goals.
Medical Eligibility & Risk Assessment
Not all patients are ideal candidates. Clinical research highlights key factors surgeons evaluate to optimize safety and outcomes.
Candidate Suitability Assessment
| Factor | Suitable | Higher Risk |
| BMI | < 30 | > 35 |
| Smoking | Non‑smoker | Active smoker |
| Diabetes | Controlled | Poorly controlled |
| Radiation history | None or planned later | Prior radiation |
| Skin quality | Elastic | Thin or damaged |
Common Medical Factors Affecting Reconstruction Choice
BMI, Smoking, Radiation, Skin Quality, Other
How Does It Work?
The surgery often happens in steps:
- Tissue Expansion (if required) involves the placement of a balloon-like device under the skin that is gradually filled with saline over a prolonged period of time to stretch the skin.
- The implant is placed under the skin or muscle during the placement of the tissue expander to complete the process.
- Later, a nipple and areola are created in order to complete the process.
Surgical Techniques & Timeline Comparison
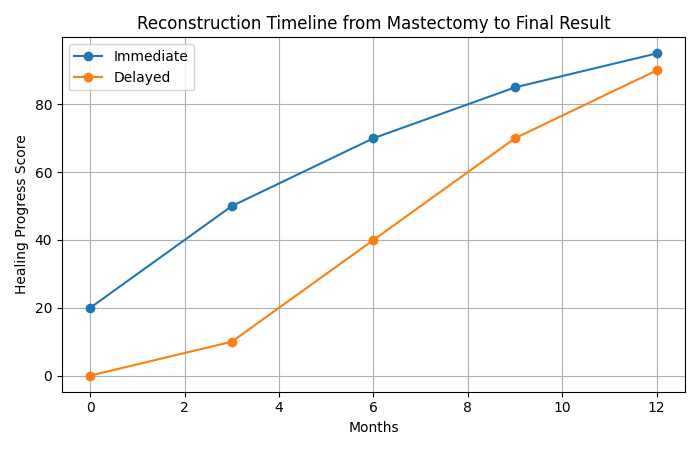
Implant‑based reconstruction can be immediate or delayed, depending on cancer treatment plans.
Immediate vs Delayed Reconstruction
| Aspect | Immediate | Delayed |
| Surgery timing | Same as mastectomy | Months/years later |
| Psychological benefit | High | Moderate |
| Impact of radiation | Higher risk | Lower risk |
| Total procedures | Fewer | More |
Reconstruction Timeline from Mastectomy to Final Result
- X‑axis: Months
- Y‑axis: Healing progress score
- Immediate vs Delayed
Choices for Implants
You pick the type with your doctor:
- Saline Implants: Filled with safe salt water. Doctors can adjust the size during surgery, and they’re cheaper.
- Silicone Implants: Filled with a soft gel that feels more like real breasts.
- Textured or Smooth: Textured ones might stop hard scar tissue from forming around the implant. Smooth ones feel softer.
Implant Safety, Durability & Scientific Evidence
Modern implants undergo rigorous testing. Large clinical studies show high satisfaction and low complication rates when monitored properly.
Implant Type Performance Data
| Implant Type | Average Lifespan (Years) | Rupture Risk (10 yrs) | Natural Feel |
| Saline | 10–15 | 8–10% | Moderate |
| Silicone | 15–20 | 3–5% | High |
Cool New Ways to Do It
Doctors in D.C. use smart tricks for better results:
Implant is placed over the muscle (prepectoral placement). There is less pain in the recovery process and you can keep using your arm muscles. Acellular Dermal Matrix (ADM) is a type of sheet from human skin (or cow or pig) that is cleaned to prevent your body from rejecting it. It functions to support and provide a natural appearance to the breast implant.
It also is supportive of the blood vessels and healing process. Fat Grafting is a process to take fat from the abdomen or thighs and place it around the implant to provide a breast that is fuller and smoother. Nipple-Sparing Mastectomy is the process of attempting to preserve the nipple and areola during the initial surgery which helps the end result to appear a lot more natural.
Advanced Technology Outcomes & Patient Satisfaction
Innovations such as ADM, fat grafting, and prepectoral placement have significantly improved outcomes.
Impact of Modern Techniques
| Technique | Pain Reduction | Aesthetic Score | Complication Reduction |
| ADM | High | High | Moderate |
| Fat Grafting | Moderate | Very High | Low |
| Prepectoral | Very High | High | Moderate |
How to Recover Well
You may experience chest pain, bruising, and swelling for a few weeks after surgery; this is completely normal. Pain medications will assist greatly. All surgeries have risks of complications, and scarring is a possibility, however doctors typically conceal scarring quite well. If there is a possibility of implant slippage, infection, numbness in the breast, or hard scar tissue (capsular contracture), risks will be reduced with good planning and an acive surgeon. It can take upwards of a year for your body to heal and your breasts to settle into their final form. The best results will occur if you follow your doctor’s orders and be as patient as you can.
Recovery Timeline & Quality‑of‑Life Outcomes
Clinical surveys show steady improvement in physical comfort and emotional well‑being over time.
Recovery Milestones
| Time After Surgery | Physical Recovery | Emotional Well‑Being |
| 2 weeks | Swelling present | Anxiety common |
| 6 weeks | Daily activities resume | Confidence improving |
| 3 months | Shape settling | Body image improved |
| 12 months | Full recovery | High satisfaction |
Top Tips for Recovery
- Stick to your doctor’s after-surgery rules.
- Take all meds on time to ease pain and fight germs.
- Skip hard exercise or lifting heavy stuff at first.
- Go to every check-up so they can watch how you’re healing.
- Eat healthy and stay active (lightly) to help your body fix itself.
Cost, Insurance & Global Access Comparison
Reconstruction access varies widely by country due to healthcare systems and insurance mandates.
Average Cost by Region (USD)
| Region | Average Cost | Insurance Coverage |
| USA | $8,000–$15,000 | Often mandated |
| Europe | $3,000–$6,000 | Public systems |
| Asia | $2,500–$7,000 | Mixed |
| Middle East | $4,000–$9,000 | Partial |
What to Expect in Washington, D.C.
In D.C., you’ll get top-notch care. Surgeons team up with cancer doctors, X-ray experts, and others for the full picture.
Costs and Planning
It costs different amounts based on the doctor, hospital, implant, and extras. Insurance often covers a lot—talk about it early. Ask your surgeon about payments too.
You’ll meet with expert plastic surgeons who know breast rebuilding. They’ll review your health, chat about what you want, and make a plan just for you.
The Good Stuff
This surgery lasts a long time. It brings back breast shape, helps you feel better about your body, and lets you wear clothes without worry. New tech makes results even better, giving hope to survivors.
D.C. has fancy hospitals with the latest tools. Plus, there are groups for talking about feelings, counseling, and help with getting back to normal life.
Implant-based breast reconstruction changes lives. It helps women heal their body and heart after mastectomy. Learn about it, ask questions, and take that step toward feeling strong again.
Long‑Term Outcomes, Revisions & Monitoring
Implant‑based reconstruction is durable, but lifelong follow‑up ensures safety.
Long‑Term Considerations
| Aspect | Data |
| Revision surgery need | 20–30% over lifetime |
| MRI/ultrasound checks | Every 2–3 years |
| Patient satisfaction (10 yrs) | ~85–90% |
Conclusion – Implant-Based Breast Reconstruction
In summary, breast reconstruction with implants after mastectomy is an effective and common way to restore the breast’s shape and symmetry. The use of silicone or saline implants makes this method less complex and provides predictable results in a shorter surgical time compared to methods requiring the use of autologous tissue.
The reconstruction of the breast after mastectomy involves multiple procedures. This approach has less tissue loss and scarring, and provides highly predictable and aesthetically pleasing results, which the patient may consider as a benefit despite the implant’s limited lifespan and the various risks and complications associated with breast implants. Implant-based breast reconstruction can greatly aid in the emotional aspect of the patient’s recovery, and with thorough planning and an experienced surgeon, the patient will receive optimal results.